Protein trends in COVID-19 patients may be a key predictor in symptom outcomes
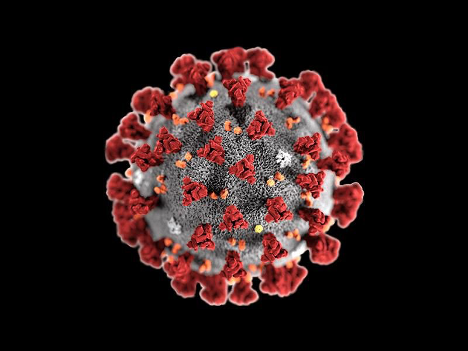
Image Courtesy of Smithsonian Magazine
November 11, 2020
Researchers at the Brigham and Women’s Hospital in Boston, Massachusetts took a keen look at a protein responsible for respiratory symptoms of COVID-19. Nominally known as the C-reactive protein (CRP), they found that a rapid rise in CRP levels within the first 48 to 72 hours of hospitalization foreshadows respiratory deterioration and intubation, while fixed CRP levels were observed in patients whose condition remained stable.
“Even though all of these patients looked clinically similar upon admission, as early as 24 hours after hospitalization, the immune systems of patients who would go on to the ICU multiple days later were already inflamed, as measured by these biomarkers,” says Edy Yong Kim, MD, Ph.D., of the Division of Pulmonary and Critical Care Medicine at the Brigham.
Physicians test levels of CRP through CRP tests, which integrate signals from cytokines, proteins that are involved in inflammation. Cytokine assays are a more specified form of testing that gives an in-depth analysis of what these cytokines tell us, especially about which proteins could be active in the inflammatory pathways. Since the results of CRP tests arrive faster than those from cytokine assays, CRP tests serve as a rational method to assess the physiological symptoms of COVID-19 patients.
These tests make a promising outlook on how to beat the odds of this virus. Kim’s summarized assessment of this protein evidence was summed up in his following quote “…a rise in inflammation directly drives respiratory failure, which implies that the immunomodulatory drugs might be able to prevent respiratory failure if given very, very early — as early as hospital Day 1 and 2.”
This study was supported by the American Heart Association Award 2014D007100 and NIAMS T32 AR007530-35.